Crushing Dread at 3 AM? Why Perimenopause Anxiety Isn’t “Just in Your Head”
Have you noticed a sudden, sharp rise in “what if” thoughts? Or perhaps you’ve started experiencing a sense of impending doom that hits you out of nowhere?
For many women in the UK, the psychological symptoms of perimenopause—specifically anxiety and panic—are far more debilitating than the physical ones. As a Registered Nurse, I want to pull back the curtain on why this happens and why you shouldn’t just be handed a packet of antidepressants and sent on your way.
The Science of the “3 AM Dread”
In perimenopause, the first hormone to take a tumble is usually progesterone. In the medical world, we often refer to progesterone as nature’s “Valium.” It is our natural anti-anxiety agent that helps us feel calm, rational, and sleepy.
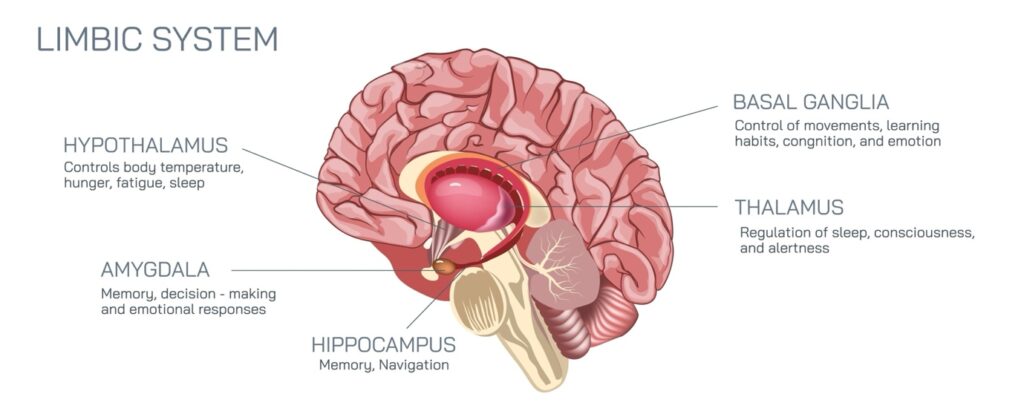
The Mechanism: When progesterone drops, your nervous system loses its natural “cushion.” This leaves your “fight or flight” response (the amygdala) on a hair-trigger. Even the smallest stressor can feel like a life-or-death emergency.
Common Symptoms:
- Health Anxiety: Suddenly becoming hyper-aware of every heartbeat or twinge.
- Social Anxiety: Feeling overwhelmed by the thought of a school run or a work meeting.
- Nighttime Panic: Waking up at 3 am with a racing heart and a mind that won’t stop spiralling.
Why GPs Sometimes Get It Wrong
The tragedy is that because these symptoms look exactly like “standard” anxiety, many women are misdiagnosed. While therapy and traditional medications have their place, if the root cause is a hormonal deficiency, you need hormonal support.
NICE guidelines are clear: HRT should be considered as a primary option for low mood and anxiety associated with perimenopause.
How to Take Control
- Reduce Stimulants: Your nervous system is already “jangly.” Cutting down on caffeine and alcohol can significantly lower the baseline of your anxiety.
- Try CBT: Cognitive Behavioural Therapy is specifically recommended by the NHS to help manage the emotional “tailspin” that hormonal shifts cause.
- Track the Patterns: Does your anxiety get worse in the week before your period? Is it linked to nights where you have hot flashes?
Don’t Walk into Your Appointment Alone
You don’t have to live in a state of constant dread. The key to getting the right treatment from your GP is showing them that your anxiety is cyclical and hormonal, not just “stress.”
Stop guessing and start tracking. Use my Perimenopause Symptom Tracker to log your anxiety spikes alongside your cycle. When you can show your GP a clear pattern of data, you move from being a “worried patient” to an “informed advocate.”
[Download the Perimenopause Symptom Tracker Here]

