The Silent Shift: Why Bone Health is the Most Important Menopause Conversation You Aren’t Having
As a nurse, I spent years working on hospital wards where I saw the “end result” of the menopause transition that no one talks about: The fragility fracture.
We spend a lot of time talking about hot flushes, mood swings, and night sweats because they are noisy and disruptive. But there is a silent shift happening deep inside your skeletal system that you cannot feel, smell, or see.
In the first five years after your final period, you can lose up to 20% of your bone density. This isn’t just about “getting older”; it is a direct result of the drop in oestrogen.
1. The Science: Why Oestrogen is Your Bone’s Best Friend
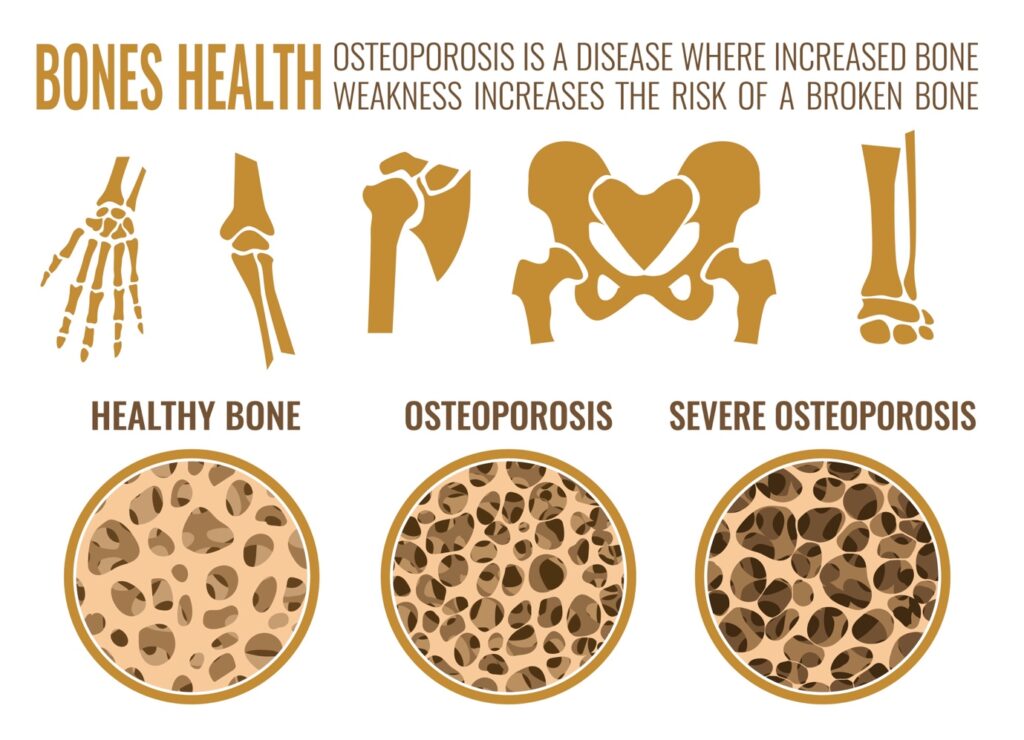
Your bones are living tissue. They are constantly being broken down and rebuilt in a process called “remodelling.”
- The Builders (Osteoblasts): These cells build new bone. They are “switched on” by oestrogen.
- The Recyclers (Osteoclasts): These cells break down old bone.
When oestrogen levels plummet during menopause, the “builders” go on strike, but the “recyclers” keep working. This leads to porous, thinning bones—a condition known as Osteoporosis.
2. The UK Reality: 1 in 2 Women
The statistics in the UK are sobering. According to the Royal Osteoporosis Society, 1 in 2 women over the age of 50 will break a bone due to osteoporosis.
The tragedy is that many women only discover they have thinning bones when they trip and break a wrist or a hip. In the nursing world, we call this the “silent epidemic” because the first symptom is often a fracture that could have been prevented years earlier.
3. The Nurse’s Action Plan: Protecting Your Future Self
The good news? Bone loss is not inevitable if you take action during the “menopause window.” Here is how we protect your mobility and independence:
A. Resistance Training (Walking is Not Enough)
While walking is great for your heart, your bones need impact and resistance to stay strong. To tell your “builder” cells to get to work, you need to lift weights, use resistance bands, or do bodyweight exercises like squats. You need to put a healthy “stress” on the bone to keep it dense.
B. The “Power Couple”: Vitamin D and Calcium
In the UK, we simply do not get enough sunlight for most of the year.
- Vitamin D: Crucial for calcium absorption. The NHS recommends everyone take a Vitamin D supplement during autumn and winter, but menopausal women should discuss their levels with a professional year-round.
- Calcium: Aim for 700mg–1,000mg a day through diet (leafy greens, dairy, fortified cereals).
C. HRT as Preventive Medicine
One of the primary clinical reasons HRT is prescribed is to prevent osteoporosis. By maintaining oestrogen levels, you keep the “builders” active and stop the rapid decline in bone density. For many women, HRT is the most effective “bone-building” tool available.
4. How to Talk to Your GP About Bone Health
If you have risk factors—such as a family history of hip fractures, a low BMI, or if you reached menopause before age 45—you have a right to discuss a DEXA scan (a bone density X-ray) with your doctor.
Don’t wait for a fall to find out where your bone health stands.
Ready to audit your risk? I’ve created a Menopause Health & Bone Density Audit. This checklist helps you identify your specific risk factors and gives you a structured list of questions to take to your next NHS review to ensure you aren’t just “managing symptoms,” but protecting your future mobility.
[LINK: Download the Menopause Health & Bone Density Audit Here]

